For US Healthcare Professionals
I am a:
TREMFYA withMe offers free resources and dedicated support for patients who have been prescribed TREMFYA®.
Supporting your patients at every step
Supporting your patients at every step

Nurse Guide* support
Specialty Pharmacy Enhanced Services
Access and affordability support
Dedicated Case Manager team
The patient support and resources provided by TREMFYA withMe are not intended to give medical advice, replace a treatment plan from the patient’s healthcare provider, offer services that would normally be performed by the provider’s office, or serve as a reason to prescribe TREMFYA®.
*Nurse Guides do not provide medical advice.
Sign-up Portal
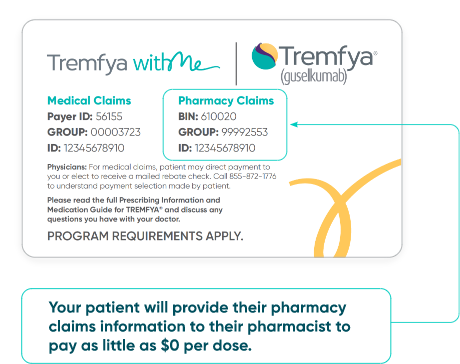
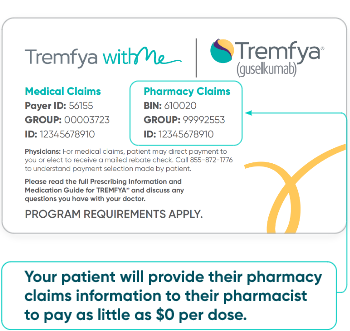
TREMFYA withMe Savings Program
Maximum program benefit per calendar year shall apply. Offer subject to change or end without notice. See program requirements at TREMFYAwithMeSavings.com
*Patients may be eligible for the TREMFYA withMe Savings Program if they are age 18 or older, use commercial or private health insurance for their prescribed TREMFYA®, and must pay an out-of-pocket cost for their treatment.
Eligible commercial patients* pay
$0
per dose
Additional Affordability Support from Johnson & Johnson
Additional Affordability Support
Patient assistance from Johnson & Johnson is available if your patient is uninsured or has commercial, employer-sponsored, or government coverage that does not fully meet their needs. Your patient may be eligible to receive their medicine from J&J at no cost for up to one year if they meet the eligibility and income requirements for the Johnson & Johnson Patient Assistance Program. See terms and conditions at PatientAssistanceInfo.com/IMM.
The patient support and resources provided by TREMFYA withMe are not intended to give medical advice, replace a treatment plan from the patient’s healthcare provider, offer services that would normally be performed by the provider’s office, or serve as a reason to prescribe TREMFYA®.
Sign-up Portal
For patients with government coverage, TREMFYA withMe can provide information about resources that may help them with their out-of-pocket costs. For a comprehensive list of affordability programs, visit
https://www.janssencarepath.com/hcp/tremfya/affordability/
Additional Affordability Support from Johnson & Johnson
Additional Affordability Support
Patient assistance from Johnson & Johnson is available if your patient is uninsured or has commercial, employer-sponsored, or government coverage that does not fully meet their needs. Your patient may be eligible to receive their medicine from J&J at no cost for up to one year if they meet the eligibility and income requirements for the Johnson & Johnson Patient Assistance Program. See terms and conditions at PatientAssistanceInfo.com/IMM.
The patient support and resources provided by TREMFYA withMe are not intended to give medical advice, replace a treatment plan from the patient’s healthcare provider, offer services that would normally be performed by the provider’s office, or serve as a reason to prescribe TREMFYA®.
Sign-up Portal
Your patients may still be eligible for support
Visit JNJwithMe.com/hcp/Tremfya to view options available for your patients.
Patients may be eligible for additional support from Johnson & Johnson
Patient assistance from Johnson & Johnson is available if your patient is uninsured or has commercial, employer-sponsored, or government coverage that does not fully meet their needs. Your patient may be eligible to receive their medicine from J&J at no cost for up to one year if they meet the eligibility and income requirements for the Johnson & Johnson Patient Assistance Program. See terms and conditions at PatientAssistanceInfo.com/IMM.
The patient support and resources provided by TREMFYA withMe are not intended to give medical advice, replace a treatment plan from the patient’s healthcare provider, offer services that would normally be performed by the provider’s office, or serve as a reason to prescribe TREMFYA®.
IN ADULTS WITH MODERATE TO SEVERE PLAQUE PsO